Is euthanasia wrong? —YES!
[EDITOR’S NOTE: This post is part of our series on controversial questions. A NO post will normally follow a YES post. Join in by posting your comments.]
by Jody Neufeld
 Euthanasia as a concept of supporting someone as they were dying is attributed to Francis Bacon in the 16th century. He wrote of helping a soul prepare vs the exterior preparation with less pain and suffering. It would be another 300 years until Dame Cecily Saunders birthed the hospice and palliative care movement. That began a global interest in medical care that included the relief of suffering in the labor of death. Interestingly, during the same time period, the development of care for working with laboring mothers also grew.
Euthanasia as a concept of supporting someone as they were dying is attributed to Francis Bacon in the 16th century. He wrote of helping a soul prepare vs the exterior preparation with less pain and suffering. It would be another 300 years until Dame Cecily Saunders birthed the hospice and palliative care movement. That began a global interest in medical care that included the relief of suffering in the labor of death. Interestingly, during the same time period, the development of care for working with laboring mothers also grew.
For over twelve years, I attended the deaths of many people in my work with hospice. Some may wonder why or how I could do this. I was honored. I learned much from my patients and their loved ones. In the early years, we were learning so much about what medications worked and what didn’t. We discovered relaxation therapies and, as medical people who are more comfortable with absolutes, we accepted that in the care of the dying, medicine was also an art, not a science. The music of Yanni might be relaxing to one patient, but the squeals and giggles of a four-year-old may also seem like music to another.
With the advancement of our knowledge of palliative care, it is my belief that the previous belief that the dying process of someone with a life-threatening illness can, and should be, a time in which “pain and suffering” is not part of the description. Yes, there are still practitioners and too many, in my opinion, government oversight bureaucrats who may spew the ridiculous rhetoric that in the care of such individuals we must be primarily concerned about pharmaceutical addition. But more commonly, physicians are embracing palliative care and working with nurses, social workers and families to provide those who are actively in their transitional journey with the physical and spiritual care they need.
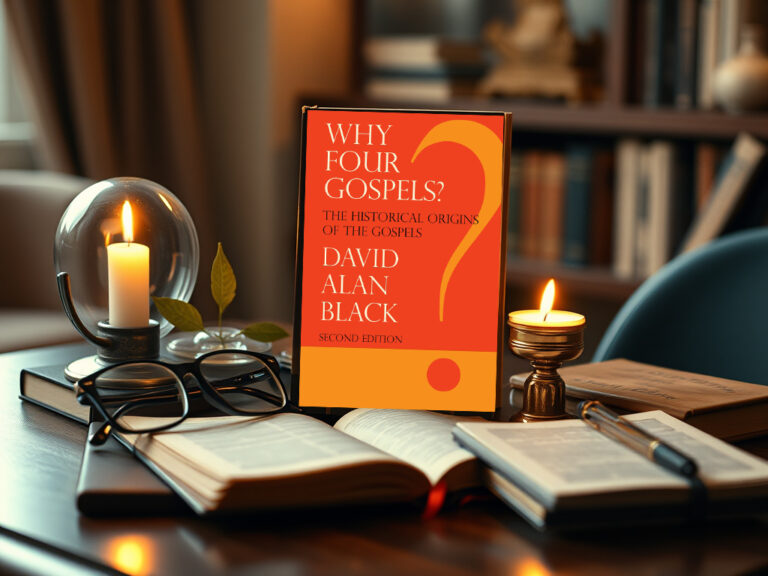
Active euthanasia is the legal tenet that is being proposed to become law. What I have discussed here so far is passive euthanasia. A patient’s decision not to seek further curative or aggressive treatment or utilize a feeding tube or antibiotics would fall under passive euthanasia. Passive euthanasia does not seek a definitive time for death but instead says, “I’m not going to prolong this journey by trying to do treatments that will not cure the underlying, primary problem.”
I read a quote from Annie Besant, a woman’s rights activist and reformer, who said it was “a duty to society to die voluntarily and painlessly when one reaches the point of becoming a ‘burden.’” It is this extreme concept that is part of the slippery slope for me in the concept of active euthanasia. Who determines when and if someone is a burden? How can euthanasia be limited to strictly a patient’s decision? What about those who are unable to verbalize their wishes or haven’t written a Living Will or signed an Advanced Directive document?
While I do believe that a person’s healthcare decisions are personal decisions, I would also submit that truly “no man [or woman] is an island.” The decision to end one’s life does have a profound effect on everyone around them. Loved ones, even when a death may be anticipated, always have regrets & wish for “just one more day.” And how would The Day be determined? Who has the wisdom to know that?
Based on my hospice years and my time with my son before he died*, I can tell you many stories that profoundly affected families and friends that no one saw coming. Not all of the stories were made for “happy ending” movies, but even the painful ones often brought people to consider their own lives in ways they could not or would not have foreseen.
By faith I believe that our Creator, Father God, gives us life and He alone has the wisdom and sight to determine the number of our days. If I had been given the power by Him as to when my son would die, would I choose 3 days, age 12, or age 15 or was that night when he was 17 the best night. I don’t know. Even in retrospect, I don’t know. I do know that even on that last night, there was laughter in memories, beauty in music and peace when I lay down in the quiet empty house. I’m not sure that would have been my description the night before. Time is such a fleeting, nebulous thing and a factor that I rarely see the point of it for good or bad when I am in the moment.
I do not believe active euthanasia is good. But loving, kind end-of-life care can be a profound spiritual experience for everyone involved.
*James was diagnosed at age 12 with rhabdomyosarcoma in his soft palate. Statistics said he had a 25% chance to survive 1 year. He received a year of chemo and radiation, 2 years of remission, another surgery then another year of remission. He did high school marching band and a season of basketball. Five years after diagnosis, cancer came back in his lung, heart, spine and kidney. He saw his niece and nephew and his brother pitch in Yankee Stadium before he died.
Loved your words, Jody. There are blessings and moments of peace at the end of death. Diane and I were sharing “death” stories and personal blessings this afternoon. Those personal blessings, we will both cherish for the rest of our lives.